The Preparation for Achievement (PAP) involves the collection and application of local painkillers, as well as clamping or gluing of the republic penile to form a protective sealing. Steps two through four involve the preparation for circumcision. These include the collection and washing of fluid and the preparation of the excretory. If pain is present, a topical anesthetic can be used. The last step, called Placenta Clamping or Neuromaxillary Clamping, is used when the successful delivery of the newborn baby has been achieved and when the newborn is free of any complications.
The steps to control infection are key to the success of neonatal circumcision. The use of an antiviral drug is one of the most important. Many of these agents have been proven to be effective in reducing HSV (herpes simplex virus) infection in children and adults. However, a University of Glasgow study showed that no reduction was seen in plasma cortisol levels in HVC-infected children or adults even after a median follow up period of two weeks. Thus, although antiviral agents may reduce the risk of neonatal herpes simplex virus (HSV) infection, the ability to reduce plasma cortisol levels 30 minutes after surgery was not present.
Circumcision can also affect blood pressure and heart rate. In the trial of Placental Clamp/Neuromaxillary along with unproven antiviral agents, heart rate decreased significantly in the placebo group given dorsal penile nerve block and control group given pacemaker. Moreover, the researchers found that after two weeks, there were significantly larger increases in heart rate in those individuals who received a pacemaker and those who received a dorsal penile nerve block. These studies have shown that circumcision has greater risks for those who need it, those who are more invasive, or those with a higher risk of developing cardiovascular disease.
CFA claims that the American Academy of Pediatrics has recommended against routinely circumcising newborns. Their claim is based on a concern that newborns are unable to physiologically withstand the pain of standard cuts made during standard infant male circumcision procedures. CFA argues that neonatal herpes risk is higher because infants are more likely to have both the rodent model virus and herpes simplex virus (HSV). The Academy has issued statements advising that there is no evidence that routine male circumcision can reduce the chances of acquiring genital herpes or measles in later years. There are three steps to circumcision Melbourne for newborns.
There are other benefits to pediatric anesthesia and surgical procedures. A study published in Pediatric AIDS Journal showed that children who had undergone traditional pediatric procedures such as circumcisions had fewer complications and more infections than those who only underwent pediatric interventions. The dorchester procedure involved the partial or full block of an infant’s dorsal perian nerve. This may not prevent a man getting H. Pylori infection but it will limit the pain and discomfort that he could feel.
CFA has some reservations regarding the risks involved in administering drugs during the procedure. In one case, they note that “a lack of scientific rigor” has allowed pharmaceuticals to be administered with little attention paid to potential drug interactions. They also point out that although many clinical trials have been done on pharmacological agents, most of them have failed to detect adverse drug reactions. Simulated disposable foreskin including an electrocauterization device has provided parents and medical professionals with better tools to manage male sexual arousal and sexual function. The method was once criticized for causing damage the penis. However, the current state-of-the-art equipment and procedure have been much praised.
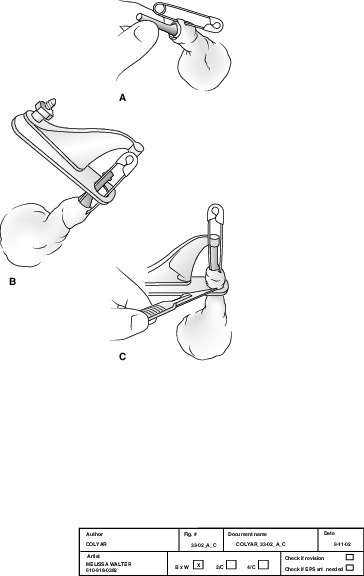
The new technique does not involve actual dilation of glans, or the removal of foreskin. However, the procedure does involve an electrocauterization device which is placed near the corona majora and the suction created by the device draws blood away from the corona majora into the glans. After about ten seconds of drawing blood, the physician then inserts a short rubber tube into the glans and drains it. The surgeon then closes the cut in preparation to remove the skin graft.
All of these steps of circumcision are performed in accordance with the recommendations of the American Academy of Pediatrics and the World Health Organization. For more information, consult your local pediatrician. There are several clinics in Florida that offer unanesthetized groups. For information on whether or not these groups are recommended by your doctor, contact the doctor or clinic.